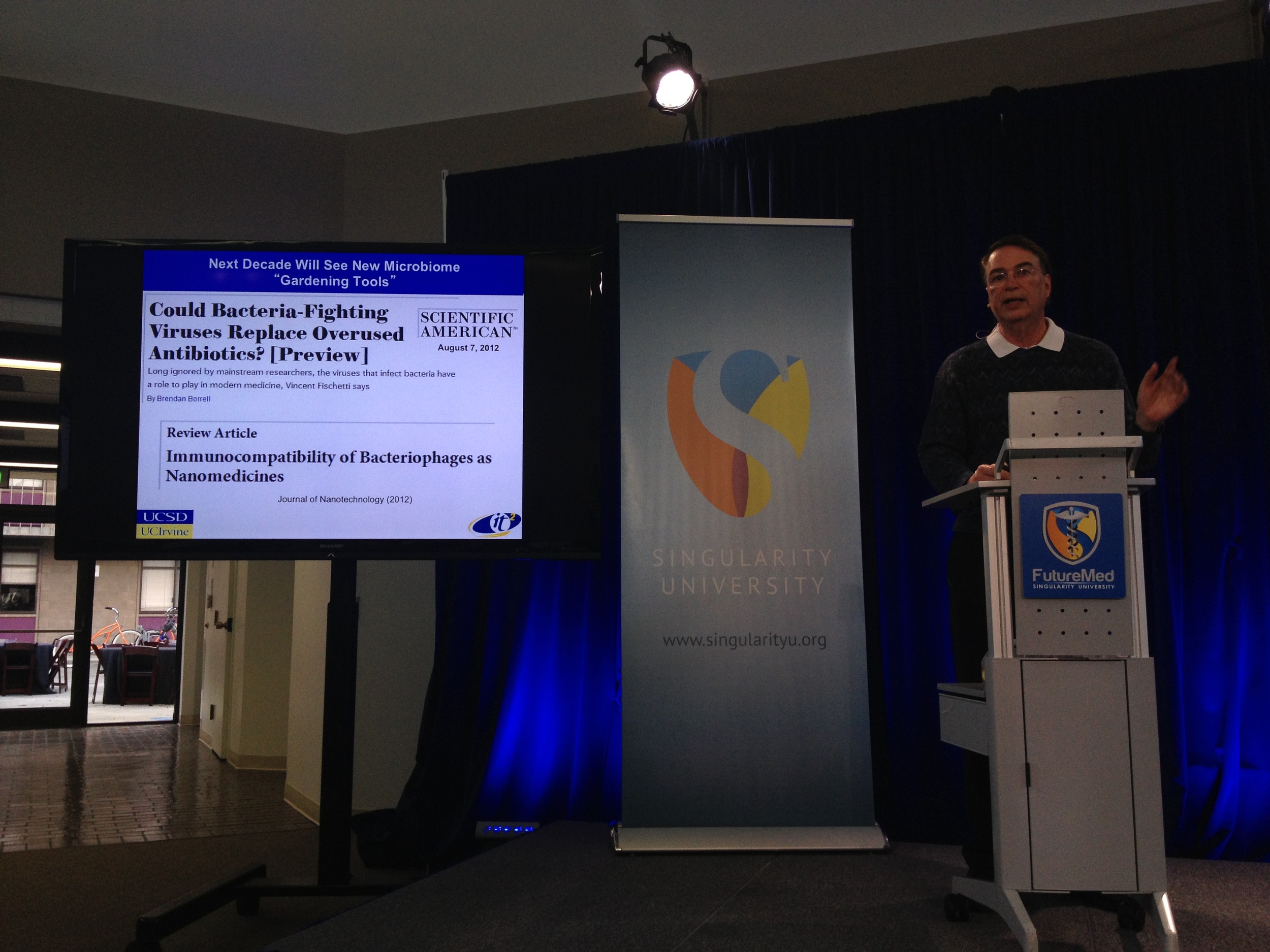
Putting patients at the heart of innovation in the NHS – Responsible or reckless?
It was fascinating to be part of the Healthcare Innovation event hosted by Westminster Forum projects last week. After the death of his wife from ovarian cancer, Lord Saatchi felt crushed by the ‘medieval’ treatment that cancer patients must endure. It drove him to launch a Private Member’s Bill in the House of Lords, which seeks to promote medical innovation and reduce doctors’ fear of litigation in the event of something going wrong. Is it right to give doctors license to experiment on their patients with unapproved treatments, even if they have the best of intentions? Is the distinction between responsible innovation and reckless innovation so easily made?
I used to think that having worked in GSK when it had approximately 100,000 employees, I’d experienced the challenges of innovating in a complex and regulated environment. However, the NHS employs more than 1.7 million people, and deals with 1 million patients every 36 hours. According to the NHS website, only the Chinese People’s Liberation Army, the Wal-Mart supermarket chain and the Indian Railways directly employ more people!
The more I learn about the inner workings of the NHS, the more respect I have for the hard working men and women who help deliver care to patients. It can be tempting to poke holes in NHS strategies from an external perspective, but I recognise that NHS leadership has to routinely make very tough decisions, particularly when evaluating the risks and benefits of new products & services.
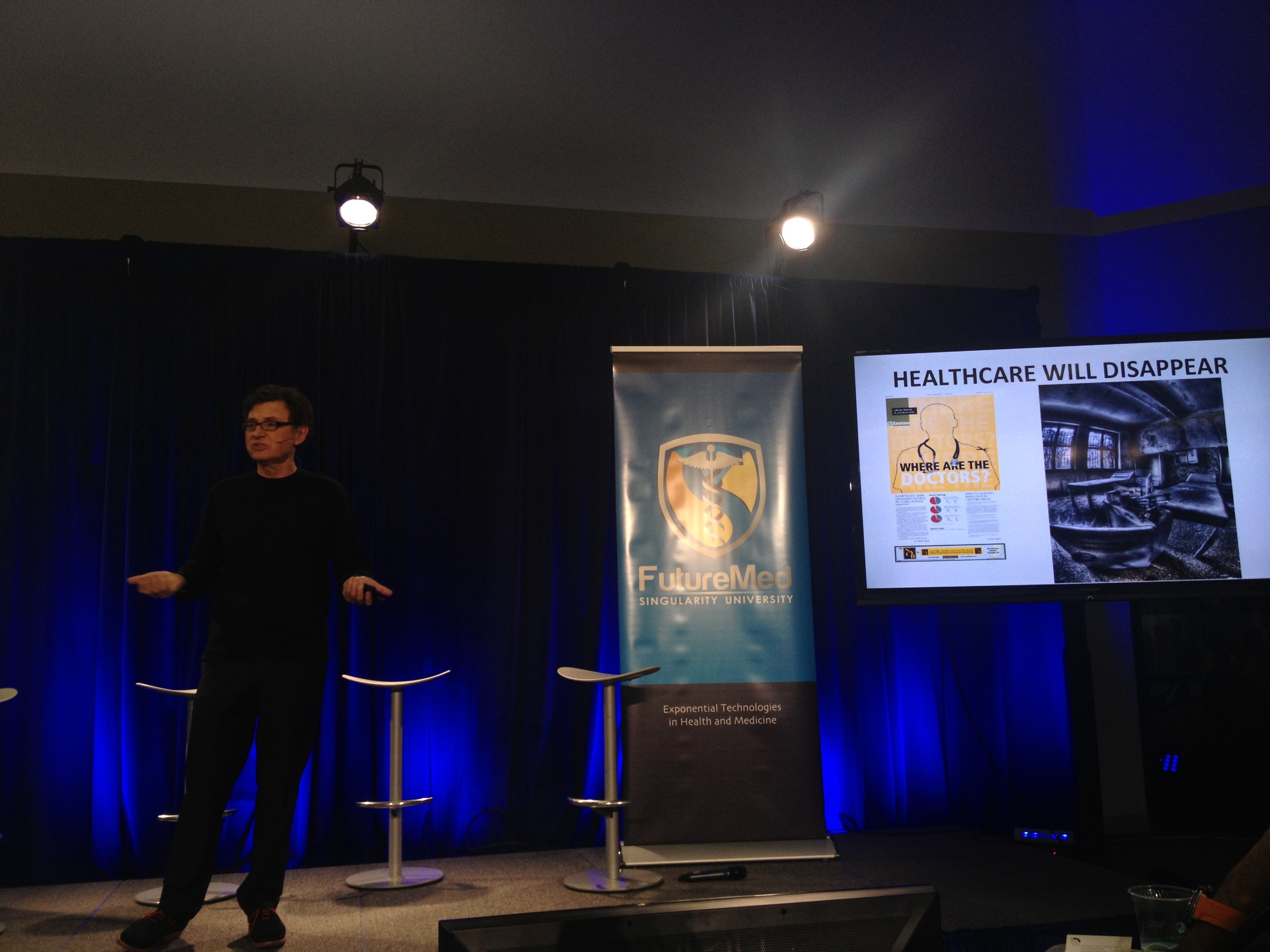
Many of the solutions we all desire for the NHS won’t arise by employing the same thinking we’ve always used. There has been significant change in recent years, and there is much more change still to come, at least from a technology perspective. When I meet innovators in Silicon Valley, they are intent on ‘disrupting healthcare’ and developing ‘algorithms’ and ‘software’ that will in theory, replace much of what a doctor does today in terms of diagnosing diseases. Then there are the multitude of startups around the globe developing mobile health apps, many of which claim to trigger ‘behaviour change’. When the pharmaceutical industry is largely focused on treatment, what will the impact be for them, if the NHS can one day use new technology to operate ‘beyond the pill’?
Indeed, Happtique in New York have been trialling prescribing health apps to patients. The Internet of Things promises us a world of billions of devices connected to the Internet, from our cars to our fridges to our clothing! Yes, the possibility of gathering streams of real-time data from a t-shirt embedded with health sensors. Google just announced the launch of Helpouts, which could one day bring telemedicine to the entire globe.
Given the biggest challenge for the NHS is chronic disease management, these advancements could make remote monitoring of the elderly a reality, except that today, 80% of care homes in the UK don’t offer internet access to their residents. 7 million people in the UK have never used the internet, many of which are poor, disabled or elderly. The Digital Divide could result in multiple tiers of innovation, not accessible to every patient.
For many people in society, these technologies could offer patients the chance to be much more in control of their health, to be more informed and to be more independent. I believe both patients & entrepreneurs will not wait for the establishment to catch up with trends in technology.
To be fair, there is a huge amount of froth and hype in Digital Health, often with limited or no evidence. There are many pioneers, but also many cowboys. The regulatory framework we use for evaluating these Digital Health technologies will have to be different from existing regulatory frameworks. We might not even get things right first time around, as this is a new area for everyone. However, we can’t let fear of failure hold us back. Many people in health & social care, particularly doctors and other leaders, are afraid at the prospect of Digital Health technologies coming into the NHS. It’s only natural to be fearful, if your own future may be at risk.
However, given a choice, I’d rather have medical professionals afraid of new technology rather than patients afraid of not having access to the latest technological innovations. Whilst we may not be able to help the patients of yesterday, such as Lord Saatchi’s late wife, I sincerely believe by continuing the open and mature debate, we could help the patients of tomorrow.
“Courage is not the absence of fear, but rather the judgement that something else is more important than fear.” - Ambrose Redmoon





















![Anthony Zacharzewski [facilitator] curating the Open Space lineup](https://images.squarespace-cdn.com/content/v1/512294dce4b03a5603ca572e/1382573027251-D4A82EZZMOF117X4DD1L/openspace.jpg)
![I think here I was describing the scale of the problem! Photo by Ruth Beattie [Yes, that's a genuine Hawaii shirt that I actually purchased in Honolulu]](https://images.squarespace-cdn.com/content/v1/512294dce4b03a5603ca572e/1382573751181-C6JZ6IC8A8PZYK3TK89E/avoid_duplication.jpg)